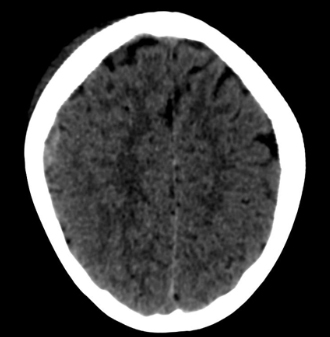
Anemia de células falciformes en imágenes de la cabeza a los pies
DOI:
https://doi.org/10.53903/01212095.320Palabras clave:
Anemia de células falciformes, Diagnóstico por imagen, Radiología, PediatríaResumen
La anemia de células falciformes (ACF) es una entidad autosómica recesiva caracterizada por la formación anormal de hemoglobina. Las manifestaciones de la ACF se deben principalmente a crisis vasoclusivas, hemólisis o infección; suele cursar con un compromiso multisistémico. En su mayoría, los hallazgos clínicos e imagenológicos son los que sugieren el diagnóstico y permiten el adecuado seguimiento. Las diferentes modalidades diagnósticas como la ecografía, tomografía computarizada y resonancia magnética desempeñan un papel esencial en la identificación de las complicaciones de la ACF. El conocimiento de las diferentes manifestaciones radiológicas específicas de la enfermedad permitirá hacer un diagnóstico diferencial correcto con otras enfermedades hematológicas, un adecuado seguimiento de esta patología y un tratamiento precoz y oportuno. Con este artículo se pretende familiarizar al radiólogo con el espectro multisistémico de la ACF en la población pediátrica.
Descargas
Referencias bibliográficas
Pinto VM, Balocco M, Quintino S, Forni GL. Sickle cell disease: a review for the internist. Intern Emerg Med. 2019;14(7):1051-64.
Piel FB, Steinberg MH, Rees DC. Sickle cell disease. N Engl J Med. 2017;376(16):1561-73.
Azar S, Wong TE. Sickle cell disease: a brief update. Med Clin North Am. 2017;101(2):375-93.
Taher AT, Weatherall DJ, Cappellini MD. Thalassaemia. Lancet. 2018;391(10116):155-67.
Steinberg MH. Sickle cell anemia, the first molecular disease: overview of molecular etiology, pathophysiology, and therapeutic approaches. Scientific World J. 2008;8:1295-324.
Nemzek WR, Swartz JD. Temporal bone: inflam matory disease. En: Som PM, Curtin HD, eds. Head and neck imaging. 4th ed. St. Louis, Mo: Mosby, 2003; pp. 1207-8.
Gladwin MT, Vichinsky E. Pulmonary complications of sickle cell disease. N Engl J Med. 2008;359:2254.
Joseph E. Maakaron, Chief Editor: Emmanuel C Besa, Sickle Cell Anemia Clinical presentation. http://www.ncbi.nlm.nih.gov/pubmed/216513. Updated: Jan 28, 2013.
Rees DC, Williams TN, Gladwin MT. Sickle-cell disease. Lancet. 2010;376(9757):2018-31.
Saito N, Nadgir RN, Flower EN, Sakai O. Clinical and radiologic manifestations of sickle cell disease in the head and neck. Radiographics. 2010;30(4):1021-34. http://dx.doi.org/10.1148/rg.304095171 .
Kotb MM, Tantawi WH, Elsayed AA, Damanhouri GA, Malibary HM. Brain MRI and CT findings in sickle cell disease patients from Western Saudi Arabia. Neurosciences (Riyadh). 2006;11(1):28-36. PMID: 22266500.
Thust SC, Burke C, Siddiqui A. Neuroimaging findings in sickle cell disease. Br J Radiol. 2014;87(1040):20130699. https://doi.org/10.1259/bjr.20130699 Epub 2014 May 21.
Allison JW, Glasier CM, Stark JE, James CA, Angtuaco EJ. Head and neck MR angiography in pediatric patients: a pictorial essay. Radiographics. 1994;14(4):795-805.
Adams R, McKie V, Hsu L, et al. Prevention of a first stroke by transfusion in children with abnormal results of transcranial Doppler ultrasonography. N Engl J Med. 1998;339:5-11.
Guy D, Bagnall R, Morgan RL, Babatunde I, Nevière A, Friedrich G, et al. Impact of transcranial Doppler screening on stroke prevention in children and adolescents with sickle cell disease: A systematic review and meta-analysis. Blood Rev. 2024; 12:101253. https://doi.org/10.1016/j.blre.2024.101253.
Ochocinski D, Dalal M, Black LV, et al. Life-threatening infectious complications in sickle cell disease: a concise narrative review. Front Pediatr. 2020;8:38.
Ginzel AW, Kransdorf MJ, Peterson JJ, Garner HW, Murphey MD. Mass-like extra medullary hematopoiesis: imaging features. Skeletal Radiol. 2012;41:911-6.
Reed Kearney P, Nasser A. Pathology quiz case 2: extramedullary hematopoeisis (EMH) of para nasal sinuses. Arch| Otolaryngol Head Neck Surg. 2002;128(1):76-9.
Berkmen Yahya M, Zalta Benjamin A. Case 126: extramedullary hematopoiesis. Radiology. 2007;245(3):905-8. http://dx.doi.org/10.1148/radiol.2453040715.
Zadeh C, Rameh V, Atweh LA. Acute soft head syndrome in a sickle cell disease patient. J Radiol Case Rep. 2021;15(4):1-6. https://doi.org/10.3941/jrcr.v15i4.4026.
Almeida A, Roberts I. Bone involvement in sickle cell disease. Br J Haematol. 2005;129:482-90.
Umans H, Haramati N, Flusser G. The diagnostic role of gadolinium enhanced MRI in distinguishing between acute medullary bone infarct and osteomyelitis. Magn Reson Imaging. 2000;18:255-62.
Collett-Solberg PF, Ware RE, O’Hara SM. Asymmetrical closure of epiphyses in a patient with sickle cell anemia. J Pediatr Endocrinol Metab. 2002;15:1207-12.
Desimpel J, Posadzy M, Vanhoenacker F. The many faces of osteomyelitis: a pictorial review. J Belg Soc Radiol. 2017;101(1):24.
Ejindu VC, Hine AL, Mashayekhi M, Shorvon PJ, Misra RR. Musculoskeletal manifestations of sickle cell disease. RadioGraphics. 2007;27(4):1005-21.
Inusa BP, Oyewo A, Brokke F, Santhikumaran G, Jogeesvaran KH. Dilemma in differentiating between acute osteomyelitis and bone infarction in children with sickle cell disease: the role of ultrasound. PLoS One. 2013;8(6):e65001. https://doi.org/10.1371/journal.pone.0065001.
Melton CW, Haynes J Jr. Sickle acute lung injury: role of prevention and early aggressive intervention strategies on outcome. Clin Chest Med. 2006;27(3):487-502, vii.
Machado RF, Gladwin MT. Chronic sickle cell lung disease: new insights into the diagnosis, pathogenesis and treatment of pulmonary hypertension. Br J Haematol. 2005;129:449-64.
Godeau B, Schaeffer A, Bachir D, Fleury-Feith J, Galacteros F, Verra F, et al. Bronchoalveolar lavage in adult sickle cell patients with acute chest syndrome: value for diagnostic assessment of fat embolism. Am J Respir Crit Care Med. 1996;153(5):1691-6.
Miller AC, Gladwin MT. Pulmonary complications of sickle cell disease. Am J Respir Crit Care Med. 2012;185:1154-65.
Kang J, Litmanovich D, Bankier AA, et al. Manifestations of systemic diseases on thoracic imaging. Curr Probl Diagn Radiol. 2010;39:247-61.
Mekki F, Taktak S, Khaldi H, et al. Acute chest syndrome as the inaugural sign of sickle cell anemia. A case report and review of the literature. Rev Pneumol Clin. 2006;62:195-9.
Vij R, Machado RF. Pulmonary complications of hemoglobinopathies. Chest. 2010;138(4):973-83. https://doi.org/10.1378/chest.10-0317.
Gardner CS, Boll DT, Bhosale P, Jaffe TA. CT abdominal imaging findings in patients with sickle cell disease: acute vaso-occlusive crisis, complications, and chronic sequelae. Abdom Radiol (NY). 2016;41(12):2524-32.
Kinger NP, Moreno CC, Miller FH, Mittal PK. Abdominal manifestations of sickle cell disease. Curr Probl Diagn Radiol. 2021;50(2):241-51.
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2025 Revista colombiana de radiología

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-CompartirIgual 4.0.
La Revista Colombiana de Radiología es de acceso abierto y todos sus artículos se encuentran libre y completamente disponibles en línea para todo público sin costo alguno.
Los derechos patrimoniales de autor de los textos y de las imágenes del artículo como han sido transferidos pertenecen a la Asociación Colombiana de Radiología (ACR). Por tanto para su reproducción es necesario solicitar permisos y se debe hacer referencia al artículo de la Revista Colombiana de Radiología en las presentaciones o artículos nuevos donde se incluyan.