Sneddon síndrome. A case presentation and review of key points
DOI:
https://doi.org/10.53903/01212095.315Keywords:
Livedo reticularis, Trastornos cerebrovasculares, Imagen por resonancia magnética, Síndrome de Sneddon, Vasculopatía, TrombosisAbstract
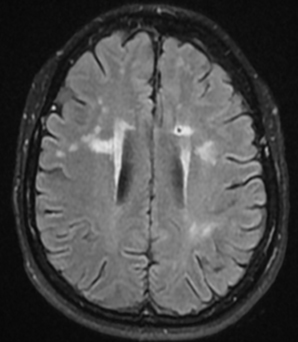
SNEDDON syndrome (SS) is a rare, non-inflammatory thrombotic vasculopathy characterized by the combination of cerebrovascular disease and livedo reticularis (LR). The estimated incidence of SS is 4/1,000,000 per year in the general population and usually occurs in women between the ages of 20 and 42 years. For the diagnosis of SS, skin biopsy and abnormal findings on neurological examination and/or magnetic resonance imaging (MRI) are mainly taken into account. Among these latter findings, it is important to highlight the presence of nonspecific multiterritorial infarcts
and cortical atrophy and, less frequently, hemorrhagic changes such as cerebral microbleeds. Angiography may reveal stenosis or occlusion of medium and large arteries and extensive networks of small collateral vessels. Previous retrospective studies on the course of the disease have revealed a wide range of neurological symptoms. We present the case of a 48-year-old woman with SNEDDON syndrome, characterized by multiple recurrent ischemic events, livedo reticularis, history of two spontaneous abortions, hypertension, progressive neurological deterioration, and a confirmed mutation of the CECR1 gene (22q11.2), who underwent a brain MRI that showed old infarcts in the bilateral centrum semiovale and basal ganglia, as well as microbleeds in the brainstem, among others. This case highlights the importance of considering SS in young patients with a history of recurrent cerebral ischemia and livedo reticularis.
Downloads
References
Wu S, Xu Z, Liang H. Sneddon’s syndrome: a comprehensive review of the literature. Orphanet J Rare Dis. 2014;9:215. https://doi.org/10.1186/s13023-014-0215-4
Boesch SM, Plörer AL, Auer AJ, Poewe W, Aichner FT, Felber SR, Sepp NT. The natural course of Sneddon syndrome: clinical and magnetic resonance imaging findings in a prospective six year observation study. J Neurol Neurosurg Psychiatry. 2003;74(4):542-4. https://doi.org/10.1136/jnnp.74.4.542
Valtchev V, Simeonova V, Gospodinov D, Yordanova I, Dimitrova V, Pavlova V, et al. Sneddon’s syndrome. J IMAB. 2008;14(1):72-5. https://doi.org/10.5272/jimab.14-1-2008.72
Kimming J. Arteriolopathie: livedo racemosa. Dermatol Wochenschr. 1959;139:211.
Champion RH, Rook AJ. Livedo reticularis. A review. Br J Dermatol. 1960;72:239-57. PMID: 13833385.
Sneddon IB. Cerebrovascular lesions and livedo reticularis. Br J Dermatol. 1965;77:180-5. PMID: 14288444.
Richard MA, Grob JJ, Durand JM, Noe C, Basseres N, Bonerandi JJ. Le syndrome de Sneddon. Ann Dermatol Venereol. 1994;121(4):331-7.
Rebollo M, Val JF, Garijo F, Quintana F, Berciano J. Livedo reticularis and cerebrovascular lesions (Sneddon’s syndrome). Clinical, radiological and pathological features in eight cases. Brain. 1983;106(4):965-79. https://doi.org/10.1093/brain/106.4.965
Hademenos GJ, Alberts MJ, Awad I, Mayberg M, Shepard T, Jagoda A, et al. Advances in the genetics of cerebrovascular disease and stroke. Neurology. 2001;56(11):997- 1008. https://doi.org/10.1212/wnl.56.11.997
Zhou Q, Yang D, Ombrello AK, et al. Early-onset stroke and vasculopathy associated with mutations in ADA2. N Engl J Med. 2014;370(10):911-20. https://doi.org/10.1056/NEJMoa1307374. Epub 2014 Feb 19. PMID: 24552297; PMCID: PMC4030999.
Frances C, Papo T, Wechsler B, Laporte JL, Biousse V, Piette JC. Sneddon syndrome with or without antiphospholipid antibodies. A comparative study in 46 patients. Medicine (Baltimore). 1999;78(4):209-19. https://doi.org/10.1097/00005792-199907000-00001 PMID: 10413707.
Schlez A, Lischka G, Schaumburg-Lever G, Ganten T, Jünger M. Raynaud symptoms as principal signs in a case of Sneddon’s syndrome. J Eur Acad Dermatol Venereol. 2001;15(4):365-6. https://doi.org/10.1046/j.1468-3083.2001.00297.x PMID: 11488836.
Wohlrab J, Fischer M, Wolter M, Marsch WC. Diagnostic impact and sensitivity of skin biopsies in Sneddon’s syndrome. A report of 15 cases. Br J Dermatol. 2001;145(3):285- 8. https://doi.org/10.1046/j.1365-2133.2001.04330.x. PMID: 11531871
Tietjen GE, Al-Qasmi MM, Gunda P, Herial NA. Sneddon’s syndrome: another migraine-stroke association? Cephalalgia. 2006;26(2):225-32. https://doi.org/10.1111/j.1468-2982.2005.01036.x. PMID: 16430634.
Ellie E, Julien J, Henry P, Vital C, Ferrer X. Divry-Van bogaert corticomeningeal angiomatosis and Sneddon’s syndrome. Nosological study. Apropos of 4 cases. Rev Neurol (Paris). 1987;143(11):798-805. PMID: 3439000.
Bruyn RP, van der Veen JP, Donker AJ, Valk J, Wolters EC. Sneddon’s syndrome. Case report and literature review. J Neurol Sci. 1987;79(3):243-53. https://doi.org/10.1016/0022-510x(87)90193-3. PMID: 3610738.
Rumpl E, Neuhofer J, Pallua A, Willeit J, Vogl G, Stampfel G, Platz T. Cerebrovascular lesions and livedo reticularis (Sneddon’s syndrome) -a progressive cerebrovascular disorder? J Neurol. 1985;231(6):324-30. https://doi.org/10.1007/BF00313561. PMID: 4003525.
Bayrakli F, Erkek E, Kurtuncu M, et al. Hemorragia intraventricular como forma de presentación inusual del síndrome de Sneddon. Neurocirugía Mundial. 2010;73(4):411-3. https://doi.org/10.1016/j.wneu.2010.01.010
Jiménez-Gallo D, Albarrán-Planelles C, Linares-Barrios M, González-Fernández JA, Espinosa-Rosso R, Báez-Perea JM. Sneddon syndrome presenting with unilateral third cranial nerve palsy. J Neuroophthalmol. 2014;34(1):50-2. https://doi.org/10.1097/WNO.0000000000000084. PMID: 24100613.
Alba MA, Espígol-Frigolé G, Prieto-González S, Tavera-Bahillo I, García- Martínez A, Butjosa M, et al. Central nervous system vasculitis: still more questions than answers. Curr Neuropharmacol. 2011;9(3):437-48. https://doi.org/10.2174/157015911796557907. PMID: 22379427; PMCID: PMC3151825.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Revista Colombiana de Radiología

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
La Revista Colombiana de Radiología es de acceso abierto y todos sus artículos se encuentran libre y completamente disponibles en línea para todo público sin costo alguno.
Los derechos patrimoniales de autor de los textos y de las imágenes del artículo como han sido transferidos pertenecen a la Asociación Colombiana de Radiología (ACR). Por tanto para su reproducción es necesario solicitar permisos y se debe hacer referencia al artículo de la Revista Colombiana de Radiología en las presentaciones o artículos nuevos donde se incluyan.