Magnetic resonance imaging findings and complications in patients with spondylodiscitis in a high complexity center in Bucaramanga
DOI:
https://doi.org/10.53903/01212095.395Keywords:
Discitis, Magnetic resonance imaging, SpondylodiscitisAbstract
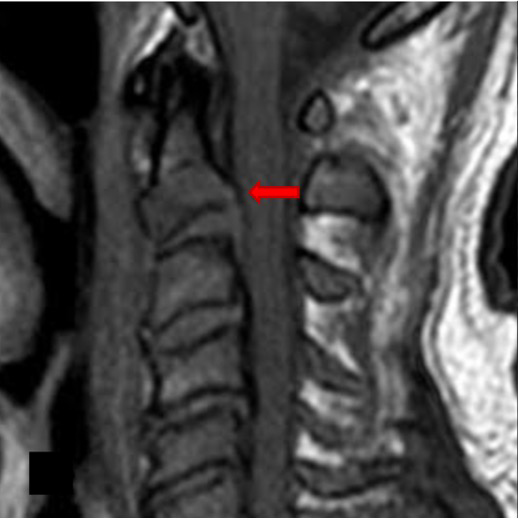
Introduction: The diagnosis of spondylodiscitis requires a high index of suspicion since symptoms and imaging findings can be variable, delayed, and nonspecific; its delay increases morbidity and mortality rates. Objective: To describe the imaging findings on magnetic resonance and complications in patients with spondylodiscitis at Hospital Los Comuneros, Bucaramanga, in the period from 2020-2023. Methodology: A retrospective, descriptive, case series study involving 21 patients diagnosed with spondylodiscitis. The frequency of positive bone biopsy cultures, magnetic resonance findings, and complications are presented. Results: The mean age was 60.2 years, with a higher prevalence in males. Magnetic resonance reported hyperintensity in the vertebral bodies, endplates, and intervertebral discs in T2 and STIR sequences with diffuse enhancement after contrast administration. In contrast to literature reports, the most frequently isolated pathogen was Staphylococcus, with greater involvement in the thoracic spine. Paravertebral abscess was present in 71.40 % of the cases, epidural abscess in 61.9 %, and spinal cord compression in 47.6%. Complications included chronic pain, pathological fracture, neurological deficit, and vertebral fusion. Conclusions: Diagnostic suspicion is crucial for timely treatment. Destruction of intervertebral endplates along with hyperintensity in intervertebral discs in T2 sequences and contrast enhancement are the most sensitive findings. Chronic pain and pathological fractures are the main complications.
Downloads
References
Kramer A, Thavarajasingam SG, Neuhoff J, et al. Epidemiological trends of pyogenic spondylodiscitis in Germany: an EANS Spine Section Study. Sci Rep. 2023;13(1):20225.
Fantoni M, Trecarichi E, Rossi B, et al. Epidemiological and clinical features of pyogenic spondylodiscitis. Eur Rev Med Pharmacol Sci. 2012;16(Suppl 2):2-7.
Formica S, Lee LA, Holtmann G, et al. Espondilodiscitis y absceso epidural por Chryseobacterium indologenes. Reporte de caso. Rev Colomb Ortop Traumat. 2022;36(2):118-23.
Couderc M, Tournadre A, Soubrier M, et al. Patología de la columna vertebral: espondilodiscitis infecciosa no tuberculosa. EMC - Aparato Locomotor. 2022;55(1):1-15.
Márquez Sánchez P. Espondilodiscitis. Radiología. 2016;58(1):50-9.
Amini MH, Salzman GA. Infectious spondylodiscitis: Diagnosis and treatment. Mo Med. 2013;110(1):80.
Herrera Camacho D. Correlación entre los hallazgos imagenológicos en resonancia magnética y el pronóstico de un grupo de pacientes con espondilodiscitis. Bogotá: Universidad El Bosque; 2020.
Navarro-Navarro R, Suárez-Cabañas AH, Fernández-Varela T, et al. Análisis de los resultados de la biopsia discal abierta y percutánea en el diagnóstico de la espondilodiscitis. Rev Esp Cir Ortop Traumatol. 2022;66(3):189-99.
Gold RH, Hawkins RA, Katz RD. Bacterial osteomyelitis: findings on plain radiography, CT, MR, and scintigraphy. AJR Am J Roentgenol.1991;157(2):365-70.
Expert Panel on Neurological Imaging; Ortiz AO, Levitt A, Shah LM, et al. ACR Appropriateness Criteria® Suspected Spine Infection. J Am Coll Radiol. 2021 Nov;18(11S):S488-S501.
Liu X, Zheng M, Sun J, Cui X. A diagnostic model for differentiating tuberculous spondylitis from pyogenic spondylitis on computed tomography images. Eur Radiol. 2021;31(10):7626–36
Naselli N, Facchini G, Lima GM, et al. MRI in differential diagnosis between tuberculous and pyogenic spondylodiscitis. Eur Spine J. 2022;31(2):431-41.
De La A, Santos CV, Juan P, Fuentes B, González Pérez F. Diagnóstico por imágenes de tuberculosis vertebral. Presentación de un caso. MediSur. 2015;13(2):303–8.
Rocha Maguey Jesús. Brucelosis espinal. Acta méd. Grupo Ángeles [revista en la Internet]. 2016.
Stoop N, Zijlstra H, Ponds NHM, et al. Long-term quality of life outcome after spondylodiscitis treatment. Spine J. 2021;21(12):1985-92.
Gouliouris T, Aliyu SH, Brown NM. Spondylodiscitis: update on diagnosis and management. J Antimic Chemoth. 2010;65(suppl_3):iii11-24.
Diagnosedaten der Krankenhäuser nach Behandlungsort ab 2000 für die häufigsten Diagnosen [Internet]. 2022 [citado: 2023 may. 30 ]. Disponible en: https://www.gbe-bund.de/gbe/pkg_isgbe5.prc_menu_olap?p_uid=gast&p_aid=92371673&p_sprache=D&p_help=3&p_indnr=550&p_indsp=&p_ityp=H&p_fid=
Marchionni E, Marconi L, Ruinato D, et al. Spondylodiscitis: is really all well defined? Eur Rev Med Pharmacol Sci. 2019;23(2 Suppl):201-9.
Harada Y, Tokuda O, Matsunaga N. Magnetic resonance imaging characteristics of tuberculous spondylitis vs. pyogenic spondylitis. Clin Imaging. 2008;32(4):303-9.
Li T, Li W, Du Y, et al. Discrimination of pyogenic spondylitis from brucellar spondylitis on MRI. Medicine. 2018;97(26):e11105.
Lee KY. Comparison of pyogenic spondylitis and tuberculous spondylitis. Asian Spine J. 2014;8(2):223.
Hopkinson N, Stevenson J, Benjamin S. A case ascertainment study of septic discitis: clinical, microbiological and radiological features. QJM. 2001;94(9):465-70.
Garkowski A, Zajkowska A, Czupryna P, et al. Infectious spondylodiscitis - a case series analysis. Adv Med Sci. 2014;59(1):57-60.
Herren C, Jung N, Pishnamaz M, et al. Spondylodiscitis: Diagnosis and Treatment options. Dtsch Arztebl Int. 2017;114(51-52):875-82.
Zarghooni K, Röllinghoff M, Sobottke R, et al. Treatment of spondylodiscitis. Internat Orthop. 2012;36:405-11.
Petkova AS, Zhelyazkov CB, Kitov BD. Spontaneous spondylodiscitis - Epidemiology, clinical features, diagnosis and treatment. Folia Medica. 2017;59:254-60.
Thavarajasingam SG, Vemulapalli KV, Vishnu KS, et al. Conservative versus early surgical treatment in the management of pyogenic spondylodiscitis: a systematic review and meta-analysis. Sci Rep. 2023;13(1).
Thavarajasingam SG, Ponniah HS, Philipps R, et al. Increasing incidence of spondylodiscitis in England: An analysis of the National Health Service (NHS) hospital episode statistics from 2012 to 2021. Brain Spine. 2023;4(3):101733.
Nasto LA, Fantoni M, Cipolloni V, et al. A Detailed analysis of clinical features and outcomes of patients with pyogenic spondylodiscitis presenting without axial back pain. Tropic Med Infect Dis. 2021;6(2):54.
Declaración de Helsinki de la Asociación Médica Mundial: Principios éticos para las investigaciones médicas en seres humanos - OPS/OMS | Organización Panamericana de la Salud [Internet]. https://www.paho.org/es/documentos/declaracion-helsinki-asociacion-medica-mundial-principios-eticos-para-investigaciones
Resolución 8430 de 1993, por el cual se establecen las normas científicas, técnicas y administrativas para la investigación en salud. Bogotá: Ministerio de Salud y Protección Social. República de Colombia (04 de octubre de 1993).
Resolución 1995 de 1999, por la cual se establecen normas para el manejo de Historia Clínica. Bogotá: Ministerio de Salud y Protección Social. República de Colombia (8 de julio de 1999).
Política de Protección de Datos Personales - Ministerio de Ambiente y Desarrollo Sostenible [Internet]. https://www.minambiente.gov.co/politica-de-proteccion-de-datos-personales/#
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Revista Colombiana de Radiología

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
La Revista Colombiana de Radiología es de acceso abierto y todos sus artículos se encuentran libre y completamente disponibles en línea para todo público sin costo alguno.
Los derechos patrimoniales de autor de los textos y de las imágenes del artículo como han sido transferidos pertenecen a la Asociación Colombiana de Radiología (ACR). Por tanto para su reproducción es necesario solicitar permisos y se debe hacer referencia al artículo de la Revista Colombiana de Radiología en las presentaciones o artículos nuevos donde se incluyan.